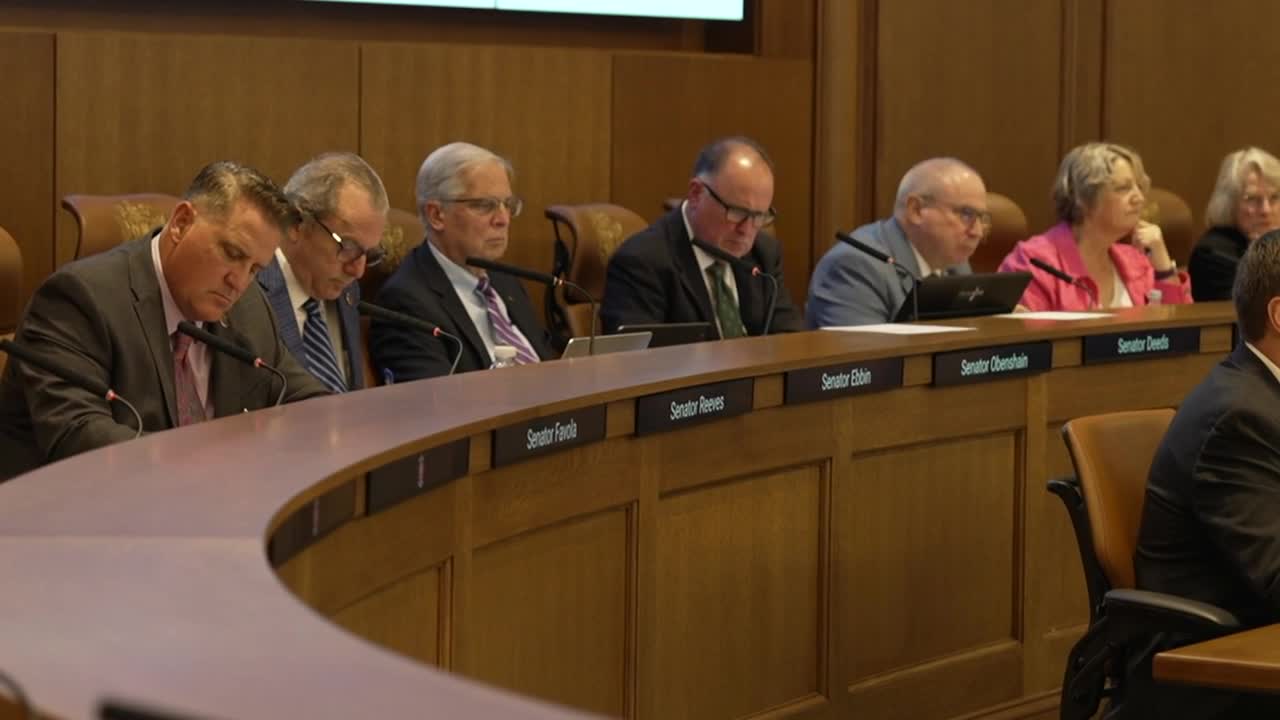
RICHMOND, Va — Why is Virginia's Medicaid agency awarding the state's lowest quality nursing homes millions of dollars in bonus payments that are meant to reward quality? That's the question some lawmakers raised during a committee meeting on Wednesday.
Their concerns followed a CBS 6 report that found the Department of Medical Assistance Services (DMAS) gave a combined $5.2 million in extra money to facilities identified by the Virginia Department of Health (VDH) as the poorest performers in the commonwealth, which are called special focus facilities.
Watch: Virginia Medicaid gave the state's worst-rated nursing homes millions in bonuses meant to reward quality
Such facilities “rarely address underlying systemic problems that give rise to repeated cycles of serious deficiencies, which pose risks to residents’ health and safety," according to the federal government, and have been cited with the most serious violations of care and safety standards over the past three years.
One of those facilities, Henrico Health and Rehabilitation Center, received more than $700,000 in value-based payments in fiscal year 2025. That fact was a shock to Senator Mark Obenshain (R-Harrisonburg), a member of the Joint Subcommittee on Health and Human Resources Oversight, which heard presentations Wednesday from VDH and DMAS on nursing home issues.
"I'm looking right now at the Medicare.gov rating for that facility, and it is so bad that it does not have any stars, and it has a notation, an exclamation point, and says this facility is not rated due to a history of serious quality issues. How on earth did that facility qualify for performance based, value-based purchasing payments?" Obenshain asked DMAS' Deputy Director Jeff Lunardi.
“It's a very fair question. The methodological answer is, they scored high enough on at least one of those metrics to earn something," Lunardi responded.
The six measures chosen by DMAS to determine whether facilities receive value-based payments include staffing levels and the avoidance of residents experiencing negative outcomes such as getting bed sores or urinary tract infections — which are mostly reported by the facilities themselves.
The higher a facility scores in those categories, or the more it improves from the previous year, the more money it gets through the program. The value-based payments are in addition to the regular base funding facilities are already receive from Medicaid, and there is no withholding of base funds in order to fund the value-based program. In total, DMAS awarded $184 million in value-based payments this past year.
Critics argue the program's methodology is flawed in part because it does not incorporate the outcomes of VDH's complaint investigations and inspections of facilities.
Delegate Mark Sickles (D-Arlington) said the value-based payments to facilities with poor inspection performances raise questions about the collaboration between VDH— the agency that inspects for care, and DMAS— the agency that allots Medicaid funding.
“Why can't you guys work better together? And if you go in and you find a nursing home that's not up to standard, do you call DMAS and say, ‘Hey, maybe you shouldn't be giving this company a value-based purchasing bonus.’ Do you do that?” Sickles asked VDH's Chief Operating Officer Christopher Lindsay.
“I saw the article that came out yesterday evening on the Value-Based Purchasing program," Lindsay responded.
“The reporter finally caught up to this. We’ve been wondering about this for a long time," Sickles said.
In Lunardi's presentation to lawmakers about value-based purchasing, he acknowledged that some parts of the program "aren't working" and that there's not enough of a difference in award amounts between facilities with high overall quality ratings and low overall quality ratings.
In 2025, data shows six other facilities with the highest possible Medicare ratings received a combined $5.9 million in value-based payments, which is not significantly higher than the combined $5.2 million received by the special focus facilities. Facilities with high Medicare ratings tend to have fewer inspection violations and better staffing levels.
"What we need to do is make sure we are rewarding the performance we want, but not rewarding those who may perform okay on one of these six measures, and so they earn something, but writ large are not the type of quality facilities we want to reward," Lunardi said.
To address that, he said DMAS is changing its framework in fiscal year 2026 to ensure that a facility that declines in performance on a certain metric will not receive a payment for that category. This change follows concerns raised by the Centers for Medicare and Medicaid Services (CMS) at the federal level that DMAS' framework allowed facilities that went backwards in a performance measure to still get a payment in that category. CMS "strongly encouraged" DMAS to stop rewarding declining performance, according to an internal memo obtained by CBS 6.
Additionally, Lunardi said DMAS will look to utilize data from VDH's inspection and oversight office in fiscal year 2027.
“As we work closely with VDH through this process, we want to look at and figure out what is the best way to use the data that they have on licensure and certification to establish whether or not there should be a core baseline or some other metric that can be brought into the value-based purchasing methodology, so that we make sure we're not rewarding facilities that are not performing up to standards," Lunardi said.
He said the agency is even considering implementing a standard that facilities will need to meet just to participate in the program. A 2022 federal study showed that "several states" with similar pay-for-performance programs did exclude nursing homes with quality issues, such as special focus facilities, from receiving quality-based payments. However, Virginia does not currently do that.
Looking at the results of the first few years of implementation of the program, Lunardi said Virginia is performing better than the national average when it comes to percentages of residents getting UTIs or bed sores in facilities. However, he said Virginia is below average when it comes to staffing levels.
CBS 6 attempted to ask Lunardi questions following the meeting, but he did not speak with us and a staffer said he was on the phone. We asked if we could talk to him after the phone call, but the staffer said he had to go. DMAS has not responded to our questions about the program that were sent on August 20.
CBS 6 did speak with VDH's Christopher Lindsay following the meeting, and he acknowledged that VDH and DMAS could do a better job of working together on this issue.
"I think this opportunity is certainly to communicate amongst all state agencies in the health sector, and this is a great example of how we could, going forward, improve communication and provide a more accurate picture to DMAS and others as far as the value-based payments," he said.
Governor Glenn Youngkin's office also responded to CBS 6's reporting on the value-based payments, a week after defending Youngkin's decision to withhold increased Medicaid funding from nursing facilities.
“This is exactly why the Governor vetoed the General Assembly’s budget amendment to provide more state funds without improvements in quality. It's why we need to reform the program and are already doing so. DMAS is currently adjusting this program to ensure that the value-based payments are reserved for facilities that demonstrate a true commitment to quality. Nursing facilities which do not meet minimum performance thresholds will no longer be rewarded. The reforms which we are undertaking will reinforce accountability and support high-quality care for Medicaid members. Only facilities that uphold or elevate their standards will be eligible for this enhanced funding, affirming our pledge to put resident outcomes and high-quality services at the forefront of our efforts," spokesperson Peter Finocchio said in a statement.
The Virginia Health Care Association (VHCA) has previously maintained that the Value-Based Purchasing program has "successfully driven performance improvements on targeted quality metrics at the provider level."
The association's president Keith Hare said factoring VDH's inspection outcomes into the Medicaid program at a time when the agency is struggling to complete timely inspections would cause disparities among providers. Hare said late inspections have already caused inequities in how Medicare distributes its overall quality ratings to facilities.
The association has long argued that Medicaid's base payments do not fully cover the costs of providing care, and Hare said in a previous interview that, even with the additional value-based payments, facilities still are not getting enough funding.
The VHCA has filed a lawsuit against the Youngkin administration's decision to withhold the increased Medicaid funding that legislators directed to take effect on July 1, 2025. The petition alleges DMAS is violating the law and the will of the General Assembly by refusing to distribute the money.
Hare said nursing homes will struggle to hire and retain staff to provide bedside care without the extra funding.
The governor's office pushed back by saying nursing homes have already received significant boosts in funding, and yet, quality of care is getting worse.
CBS 6 is committed to sharing community voices on this important topic. Email your thoughts to the CBS 6 Newsroom.
📲: CONNECT WITH US
Blue Sky | Facebook | Instagram | X | Threads | TikTok | YouTube