RICHMOND, Va. — Virginia's Medicaid agency awarded the state's lowest quality nursing homes millions of dollars in bonus cash meant to reward quality. While critics point to that fact as proof the program is doing very little to actually improve quality of care in facilities, the industry maintains the program is successful.
Cynthia Jefferson's first thought was one of shock after learning her aunt's nursing home Henrico Health and Rehabilitation Center received more than $700,000 this past year in extra taxpayer funds from the Department of Medical Assistance Services (DMAS), which oversees Medicaid in Virginia.
The money came through a program that "strives to reward quality and to support improvement."
“Where's the money going? The food looks like slop. If you're getting that type of money, then you at least should feed these people a proper meal," Jefferson said. “Medicaid and Medicare need to hold these people accountable first of all."
The thing is — Henrico Health and Rehab has been identified by the Virginia Department of Health (VDH) as the lowest-rated, worst-performing nursing home in the state, which is called a special focus facility.
Watch: Henrico nursing home identified as one of the worst care facilities in the country
Special focus facilities “rarely address underlying systemic problems that give rise to repeated cycles of serious deficiencies, which pose risks to residents’ health and safety," according to the federal government.
Medicare ratings warn that Henrico has been cited by inspectors for abuse, and past inspections have revealed violations for neglecting incontinence care, sexual abuse by staff against residents, and insufficient staffing levels.
“I don't think they should be getting a reward. Nobody should get a reward if they're not up to standards. You’re setting a bad example," Jefferson said.
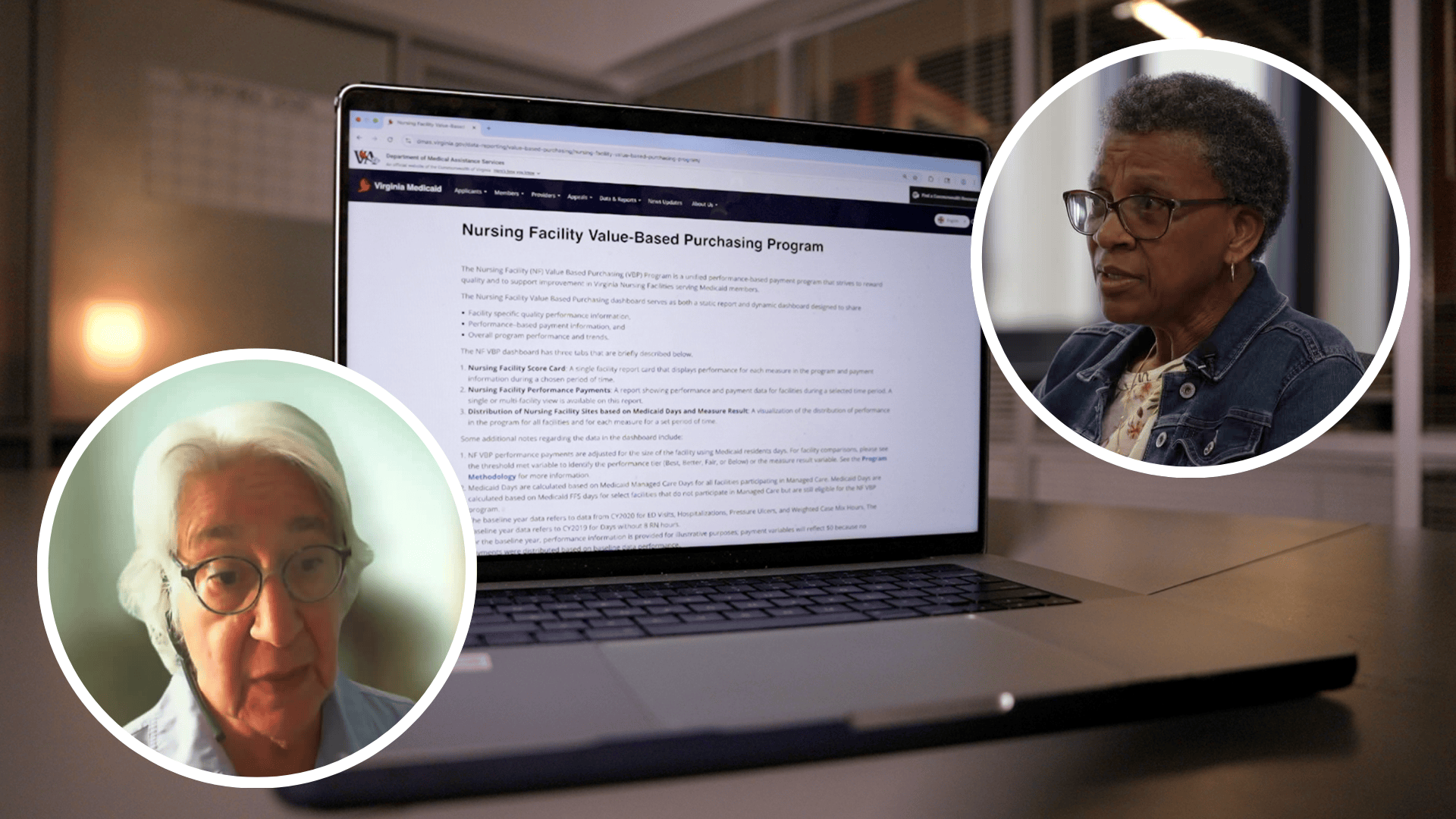
DMAS was directed by lawmakers in 2021 to establish its Value-Based Purchasing (VPB) Program in an effort to incentivize nursing homes to provide better care to Medicaid patients.
Here's how the program works: DMAS collects data, mostly reported by the facilities, on staffing levels and the avoidance of residents experiencing bad outcomes like getting bed sores or urinary tract infections.
The higher a facility scores in those categories based upon the data it submits, or the more it improves from the previous year, the more money it gets. The payment amounts are determined by a tiered system offering varying financial incentives at each level.
These value-based bonus payments are distributed in addition to the regular funding facilities already receive from Medicaid. DMAS does not withhold any base payments from facilities in order to fund the program.
But critics, like Toby Edelman with the Center for Medicare Advocacy, argue programs like this don't actually achieve their goals of increasing quality.
“They're not really making a difference. It's like money just being given to facilities and not reflecting really significantly better care or much of anything. It’s just, 'We're going to give you some more money,'" Edelman said.
Take for example: Henrico Health and Rehab and the five other special focus facility candidates.
Through the last three years of inspections and complaint investigations, VDH has found that these nursing homes have shown a pattern of committing the most serious violations of care and safety standards.
And yet, DMAS gave them a combined $5.2 million in value-based payments in fiscal year 2025.
“Why would these facilities be getting extra money for providing good care when the other part of the state is saying, ‘These are the worst facilities in the state’?” said Edelman, an expert in nursing home regulation. "These are facilities that have very serious deficiencies for a very long period of time. It's not just like one thing went wrong one day. These are really poorly performing facilities, and the candidates meet the same criteria."
The special focus facilities' combined $5.2 million in performance payments were not much lower than the combined payments of $5.9 million awarded to six other facilities with the highest possible overall quality ratings from Medicare.
In contrast to special focus facilities, nursing homes with the highest possible Medicare ratings tend to be cited with much fewer violations during inspections and tend to have better staffing levels.
Edelman said the awards to poor performing facilities raise questions about the metrics chosen by DMAS to determine its value-based payments. She said a majority of its selected metrics rely on unaudited data reported by the facilities themselves.
A federal study released in 2022 showed "several states" with similar pay-for-performance programs excluded nursing homes with quality issues, such as special focus facilities, from getting value-based payments — but Virginia does not do that.
Virginia's program also does not take inspection results, including the scope and severity of regulatory violations, into consideration. But the Virginia Health Care Association (VHCA), which represents the industry, suggested that may actually be a good thing.
Because the Virginia Department of Health is so behind on completing inspections of facilities, VHCA president Keith Hare said factoring inspection outcomes into the Medicaid program could create inequities among providers. Late and untimely inspections have already caused disparities in how Medicare distributes its overall quality ratings, he said.
The organization noted Medicare's quality rating system is not a direct comparison to Medicaid's Value-Based Purchasing program as they rely on different metrics and inputs.
"VHCA-VCAL strongly supports the VBP program, which was developed to enhance Medicaid funding for nursing facilities. While no program is without its challenges, VBP has successfully driven performance improvements on targeted quality metrics at the provider level," Hare said in a statement.
The industry has long argued that Medicaid's base rates do not fully cover the costs of providing care.
In an interview with CBS 6 last week discussing a lawsuit filed by nursing facilities against Governor Glenn Youngkin's administration over the withholding of increased Medicaid funding, Hare said the value-based payments still aren't enough to support providers' needs.
Watch: Nursing homes sue Virginia over alleged failure to provide increased funding for direct care
“We need every single bit of funding we possibly can. Nursing homes have been underfunded, really nationally, but also in Virginia, for over 30 years," Hare said.
Defending the decision to withhold funding, Youngkin's office said in a statement last week that nursing facilities have already received significant boosts in funding, including through the Value-Based Purchasing Program, and yet quality of care is getting worse, not better.
Edelman argued that while it's true some facilities may not receive enough Medicaid funding to fully cover costs, it's "not true across the board." She said a lack of financial transparency and inadequate information about related-party transactions, which occur when facilities pay other companies under common ownership for services, make it difficult to track how money is spent.
"Until we know about related parties, we can't say [nursing homes] don't get enough [funding]," Edelman said.
Even based on the Value-Based Purchasing program's existing performance measures, the Centers for Medicare and Medicaid Services (CMS) has said it's concerned that DMAS' award framework allows a nursing facility that worsens on a metric to still get a value-based payment.
According to an internal memo dated July 2025 and obtained through a public records request, CMS questioned DMAS about how its proposed fiscal year 2026 methodology complies with regulatory requirements of only giving payments to facilities that demonstrate maintenance or improvement in a performance category.
For example, Virginia's program still pays a facility that happens to decline on a performance metric as long as it doesn't drop to the lowest possible tier. According to the memo, CMS "strongly encouraged Virginia to explain how it will... limit payments to [nursing facilities] with declining performance."
CBS 6 asked DMAS on August 20 how it's responding to CMS' concerns and whether it believes the program has been successful in improving quality of care. We still have not received a response.
In her opinion as the family member of a resident, Jefferson said the volume of complaints and inspection violations should determine whether a facility gets value-based payments. And when facilities don't show improvements, she said Medicaid should "stop paying."
“You’re getting ample enough dollars, and you're not utilizing it in the right place. So why do you need a bonus?” Jefferson said. "Medicaid should be accountable for what they do. Know where the money is going and why."
CBS 6 is committed to sharing community voices on this important topic. Email your thoughts to the CBS 6 Newsroom.
📲: CONNECT WITH US
Blue Sky | Facebook | Instagram | X | Threads | TikTok | YouTube