RICHMOND, Va. — New research published by a group of pharmacists is raising concerns about Virginia's reported overspending on drugs for Medicaid patients. However, the state is pushing back against the findings, citing inaccurate spending data that it has been submitting to the federal government for several years.
The report was done by Strategic Directions Rx, a healthcare consultant group, and Pharmacists United for Truth and Transparency, an organization that advocates for independent pharmacists.
The report's author, pharmacy owner and data analyst Jeremy Counts, said the findings indicate a troubling trend of the Department of Medical Assistance Services (DMAS), the state Medicaid agency, reportedly overpaying for medications at pharmacies and outpatient facilities.
“We've got elevated spending on prescription drugs to levels that are obscene, but we've got pharmacies closing down everywhere. We've got providers who can't stay open because they're getting under-reimbursed," Counts said. “It's alarming, and we've got to get a hold on it right now, or things are going to get much, much worse.”
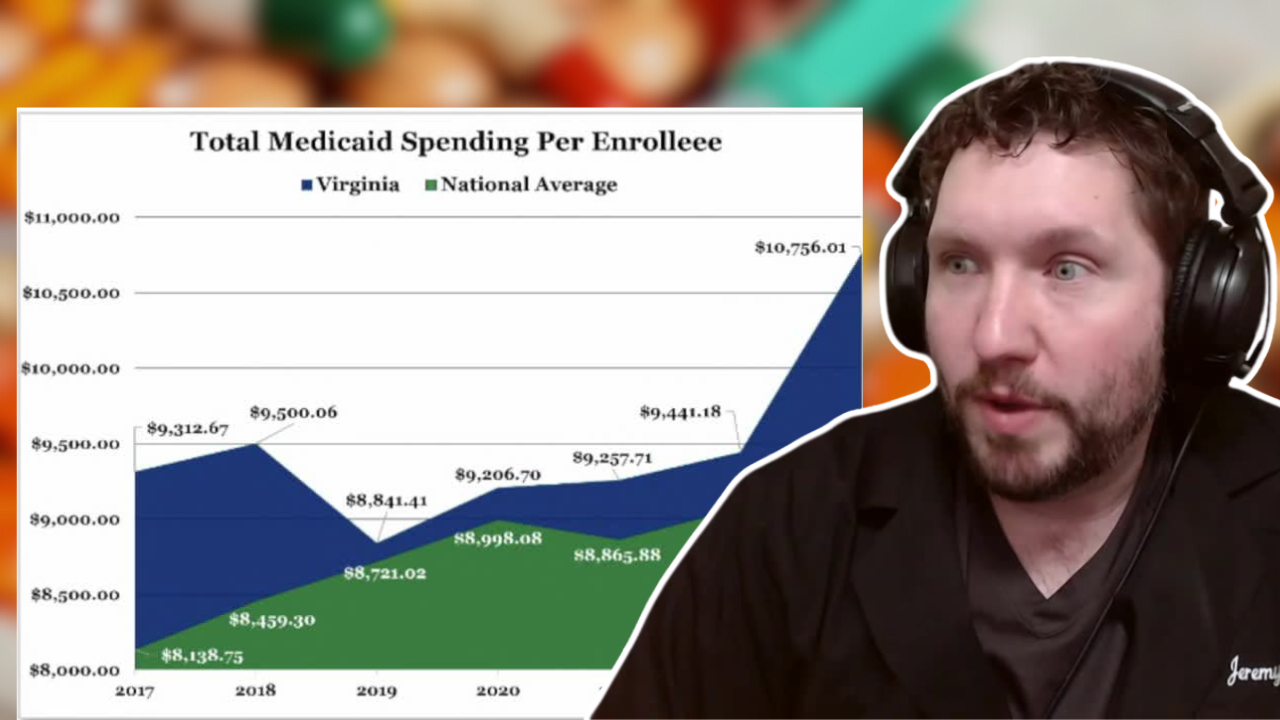
Counts analyzed data that DMAS submitted to the Centers for Medicare and Medicaid Services (CMS) from 2017-2023. During that time, he found Virginia reportedly overspent by $10.86 billion on drugs compared to other states.
In 2023 alone, he concluded Virginia reportedly spent roughly $2,600 on drugs per Medicaid enrollee, which was four times higher than the national average of $555.
“If we do not fix this problem, we are going to see drug spending continue to increase and increase and increase while Virginia does not have that kind of money," Counts said.
However, the state countered that Counts' research is based on flawed data that DMAS has been filing inaccurately four times a year beginning in 2019.
In a statement, DMAS spokesperson Kedra Keith said the data includes “inflated claims pricing for prescription drugs dispensed in non-retail settings” such as hospital claims that are paid in bundle payments.
As to what caused the error, Keith blamed an “incorrectly coded data extraction.”
“It still has to be signed off on quarterly, and this has been happening since 2019, so this is really alarming, and right now, the taxpayers deserve to know, have answers," Counts said.
Even still, Counts argues inflated cost data is a big issue, because he said it's used for research purposes that affect policy and the rates that Medicaid pays to health plan organizations to cover the costs of drugs.
“Whether they're saying that it's inflated or not, that's irrelevant when it ends up impacting what we spend overall for medications," Counts said.
DMAS provides capitation payments, which are essentially monthly premiums to cover drug costs, to managed care organizations (MCOs), which then contract with pharmacy benefit managers (PBMs), which then negotiate costs and reimburse pharmacies.
However, Counts said MCOs and PBMs are sometimes under common ownership, and in those cases, he said they're "contracting with themselves" and the money "is passing through multiple layers of the same company."
Viginia's Attorney General Jason Miyares has joined other attorneys general across the country in pushing for PBM reform measures. One letter he signed last year said PBMs "have only made the pharmaceutical market more opaque and have been a cause of rising drug prices" and make it difficult for independent pharmacies to survive.
This year, Governor Glenn Youngkin signed a law that will require DMAS to contract with one PBM in a move that supporters say will ensure more transparency around spending and savings — a solution that Counts highlighted in his report.
In a letter to Counts, Virginia's Health and Human Resources Secretary Janet Kelly blasted his report as "neither truthful nor transparent," and she requested a retraction.
"We share your commitment to lowering prescription drug costs and improving health care for all Virginians and we hope you will honor that shared goal by ensuring your analysis is based on accurate and reliable information. As I am sure you know, the validity of research findings is only as strong as the quality of the data on which they are based; flawed data will inevitably yield flawed conclusions," Kelly wrote.
Counts told CBS 6 he stands by his report and continues to wait for DMAS to provide the corrected data.
A CMS spokesperson said the data at the center of Counts' report is primarily used to facilitate the rebate process between states and drug manufacturers, adding "states may need to make corrections to ensure rebate collections are accurate, but financial adjustments are generally handled at the state level with manufacturers."
CBS 6 asked DMAS to confirm whether the incorrect data caused the agency to receive rebates it should not have, and we are still waiting for an answer.
CMS said it has authority to conduct a review of state rebate programs when "accuracy issues" are identified but did not directly answer whether it was taking such action with Virginia.
CBS 6 is committed to sharing community voices on this important topic. Email your thoughts to the CBS 6 Newsroom.
📲: CONNECT WITH US
Blue Sky | Facebook | Instagram | X | Threads | TikTok | YouTube